Finding a Breakthrough for Tucker and the World
NICHD study on Niemann Pick Disease Type C has been making discoveries since 2006
Here at The Children’s Inn at NIH, we pride ourselves on being “A Place Like Home” for children, teens, young adults, and their families. Sometimes, the child, teen, and young adult are all the same person. Such will be the case for Tucker, a 15-year-old from Strawberry Point, Iowa who has been coming to The Inn since he was six months old.
Tucker was born with Niemann Pick Disease Type C (NPC), a rare genetic storage disorder which can cause serious damage to the nervous system over time. His parents are both carriers of this inherited disease but were unaware of it as it did not present in any of Tucker’s three older step-siblings.
When Tucker was born jaundiced, the condition did not improve as quickly as his doctors would have liked. By the Spring of 2009, when he was four months old, he developed pneumonia which sent him back into the hospital twice. Eventually his local doctors referred him to the University of Iowa Stead Family Children’s Hospital.
“We were fortunate and unfortunate,” remembered Tucker’s mother Barb. “When we went to the University of Iowa Stead Family Children’s Hospital, there are only about 600 cases in the world and the doctor that we saw diagnosed her first case of NPC in September of 2008. Tucker was there in April 2009. To have one case in your career is extremely rare. To have two is almost unheard of.”
Tucker had an enlarged liver and spleen as a result of NPC, which pushed on his lungs and, at least in part, led to the pneumonia. Once the official diagnosis was in, Tucker benefited from his doctor’s experience as he was quickly referred to NIH, where a study was ongoing that his doctors had learned about after their prior experience. By Memorial Day of 2009, when he was six months old, Tucker arrived at The Children’s Inn.
“It’s all overwhelming when you first get this diagnosis,” said Barb. “You’re traveling for the first time with a six-month-old and all of that. But it was a good experience when we were there. Everybody was friendly. When we come, it seems like we always meet other families from around the world, and the staff has always been helpful. The people there made it a great experience.”
One of the first tests Tucker underwent at NIH was a spinal tap. Barb remembers being terrified of sending her baby off for this difficult procedure. “They took him out of the room, and he was sleeping when he left, and he was still sleeping when they came back,” she laughed. “So, I felt a little better after that.”
The problems caused by Tucker’s NPC as an infant were serious but could be handled. When he was diagnosed, though, his parents were warned that by age two, many NPC patients start to develop more serious symptoms, sometimes including death. Typically, NPC ends up taking over the brain, causing neurons to die and ultimately shutting down the ability to function.
“But he met that two-year-old marker with no symptoms,” laughed Barb. “So, then we got to the five and six-year-old and said that that’s probably when we’ll get symptoms. We hit that and still no symptoms, and now we’re all the way up to 15 and we really don’t have any symptoms either. So [his doctors at NIH] are just kind of looking, watching him, following him to see if symptoms arise. Since he hasn’t had any symptoms, he’s a very rare case. And they will tell you that they’ve never had someone that they’ve seen for 15 years that has basically had no symptoms.”
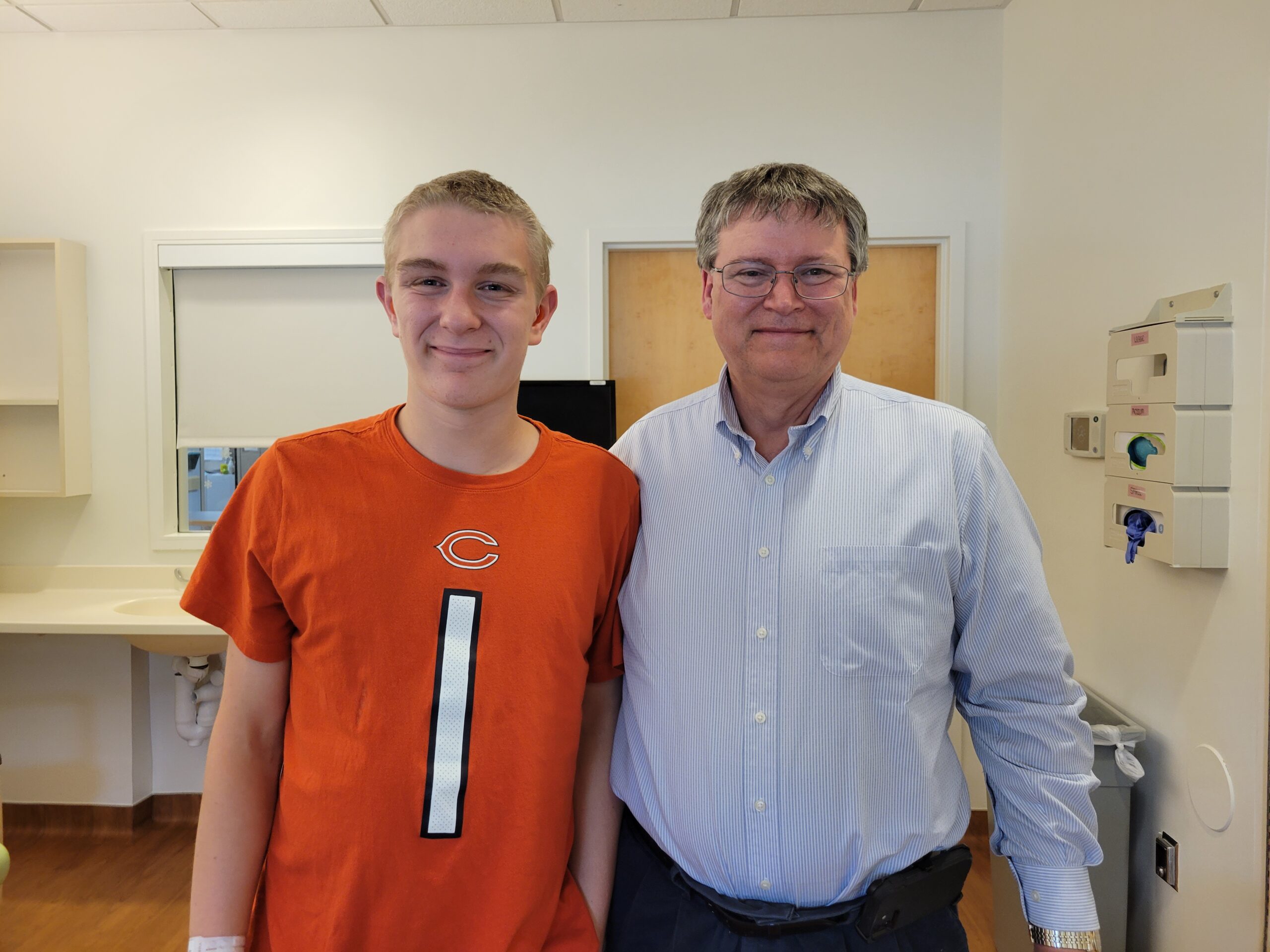
Tucker’s lead doctor is Dr. Forbes Porter, a Senior Investigator at the Eunice Kennedy Shriver National Institute of Child Health and Human Development. He met Tucker as an infant and enrolled him in his natural history study of NPC.
In natural history studies, researchers examine how a disease or medical condition develops over time. Researchers follow participants who are at risk for or have a specific disease or condition to determine how specific factors, such as family history, age, and occupational exposure, affect the development or progression of the disease or condition. Data collected during a natural history study also provide information on how best to treat a condition or disease.
“The natural history study was set up in 2006 and its initial goals were to determine if we could identify outcome measures [for NPC],” Dr. Porter explained. “It also had the goal of identifying a biomarker that could simplify the diagnosis, and we’ve been able to accomplish that.”
Since its initial success, the protocol has been expanded to try to understand more about the disease. “NPC is very heterogeneous,” he said. “All the patients are different. The age of onset is different. I have babies that are severely affected and then you have adults and people like Tucker who may have spleen and liver problems as an infant but are now doing well. So we’ve expanded the study to include obtaining genome sequencing to try to identify modifier genes in a well-described population. The purpose now, really, is to identify tools that will facilitate therapeutic trials.”
Since coming to NIH for the first time back in 2009, Tucker has been on a drug called Miglustat. It inhibits the glycosphingolipids that accumulate in NPC, slowing their accumulation. Approved in much of the world for treatment of NPC, Miglustat is still not approved by the Food and Drug Administration in the United States because of the exacting testing standards required by that organization, standards difficult to meet with a disease as rare and serious as NPC.
“Tucker is not on any experimental therapies,” Dr. Porter clarified. “But most physicians who deal with NPC consider [Miglustat] to be the standard of care now.”
Dr. Porter’s study is open-ended, meaning that it will continue searching for more information on NPC even as the questions it poses get answered over time. Tucker is one of 148 members of the study, which relies not only on a small network of doctors around the world who work with NPC but also on social media and the interconnectivity of the families afflicted with it.
“Parents get this diagnosis, and it can be devastating,” Dr. Porter explained. “They Google support organizations, and that word of mouth helps potential patients hear about our study.”

Tucker playing pool at The Inn
Tucker is able to live his daily life without many reminders of his diagnosis. He has played football, basketball, golf, and ran track for his school. He also does Taekwondo, something Barb describes as “unheard of” for a 15-year-old with NPC. He still has an enlarged spleen and liver, but nothing else that doctors can tie to the NPC. Though he suffers from hearing loss and had to have surgery for a crossed eye recently, neither issue is something his doctors can definitively say stems from his genetic disease.
Should his disease progress in a more aggressive way, Dr. Porter holds out the possibility of moving Tucker onto more experimental treatments within the framework of the study. But for now, the Miglustat is working, and Tucker is serving a critical role in helping Dr. Porter and others understand more about NPC.
“It presents in different ways and progresses in different ways in different kids,” Barb said. “So, they can study Tucker to find out more about it and why he is doing so well. They can find the biomarkers and things that caused this disorder in the first place.”
In the meantime, Tucker continues making regular visits to The Children’s Inn. And throughout his journey from child to teenager and soon to young adult, The Inn has been a place where Tucker can find comfort and fun, and a little bit of the mischief that comes with childhood.
“When he was three, we were up in the playroom and he was coming down from the treehouse there,” Barb remembered. “I had warned him about three times not to jump down the stairs, but he was jumping. He jumped down off the bottom step and turned to look at me and lost his footing, and he fell face-first and knocked out his three front teeth. We had to go by ambulance across the street to the hospital so we could get it looked at. He knocked them completely out, roots and all.”
“He’s a teenager now,” Barb smiled. “He’s graduated from the playroom to the outside playground to the video game lounge. The last time we were there, he really enjoyed the teen room.” To date, no other teeth have been lost on the grounds of The Children’s Inn. As he has gotten older, he makes a point to help the younger kids he sees at The Inn feel as comfortable as he once did.
“He’s very good with young children,” Barb said. “A lot of times I see him talking to kids. He’s got a nephew who is five and takes to him like glue. He is so good with the younger kids.”
The Inn will continue to be there for Tucker and many other families involved in Dr. Porter’s study and others like it. By creating “A Place Like Home” for these children, teens, young adults, and families, The Inn is a vital partner to doctors and scientists like Dr. Porter making life-saving breakthroughs every day at the NIH.




